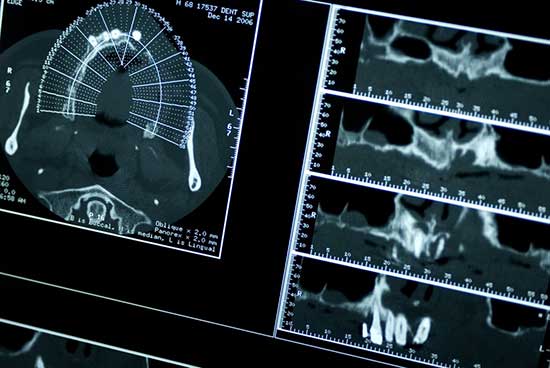
Dental radiography has enabled surgeons to save teeth and learn about dental anatomy for over a century. While X-rays and other penetrating wavelengths were still being researched and discovered, dental experts had already started applying them into non- invasive exploration of tooth internals. The ability to take a look inside a tooth while it is still viable gives dentists the information they need to decide what to do with the tooth and how to approach it.
The fact X-ray radiography is still with us since the days of the First World War only emphasizes on what a great discovery it is.
However, records are made to be broken and what was the first candle to enlighten the journey into the core of our bones is being supplemented by a bright projector.
One of the major concerns with X-ray is radiation, which ionizes atoms inside the cells, causing breakage of proteins into radicals, which are then picked up into the DNA structure, yielding single-strand breakage (usually repairable by the cell, which uses the good copy) or double strand breakage (which cannot be repaired). Cells with mutated DNA are with much shorter life, in the best case. In the worst case, they don't die but rather multiply uncontrollably, a phenomenon called Cancer.
Luckily, avant-garde usages of light provides new ways to diagnose bone problems.
Optical Coherence Tomography (OCT) gives surgeons a tool they can use repeatedly without putting the patient at risk.
The utilization of near-visible infra-red light is especially valuable because, at that wavelength, enamel is pretty much transparent and a similar effect to X-ray is achieved, albeit limited to enamel (excluding dentine and gum tissue).
Like the X-ray, this is an invention that's being put to use well before it has matured. Researchers are still finding out new ways to cash in on the benefits of light.
One promising methodology is the heuristics of pathological conditions. This is essentially a return to the era before X-rays, with a twist.
Back in the days, a dentist had to examine a tooth and tell from the outside whether it is good or bad. Similarly, a surface image or cross-enamel scan does not tell the surgeon the condition of the root but the enamel is almost always a projection of the underlying infrastructure and disrupted patterns in it indicate the availability of a condition.
This is only very effective because of the penetrating and high-resolution capabilities of OCT devices.
In order for the resulting projection to be seen by the human eye, the infra-red light needs to be “painted” with visible colours. This requirement inspired the inventors to apply a whole colour palette: healthy tissue is coloured as usual – inflamed tissue can be contrasted using, for example, violet. The same contrast can be applied to other problems: puss, lesions, cracks, caries and even to differentiate natural from prosthetic tissue (a white filling, for example). This contrasted view of the materials can be taken in real time, while the surgeon is excavating and that means the surgeon knows exactly where and how much to remove – keeping more natural, healthy tissue with the patient.
The enhanced resolution possible with OCT opens a path for advanced image processing to kick in. Software is thus able to deduct a 3D model from the pictures of the teeth, sculpturing a virtual mouth which can be shown to the patient, surgeon and his colleagues (via PACS) and, in that way, examine the mouth from angles unobtainable physically, contributing to more accurate manufacturing of prosthetics, which directly translates to less suffering to the patient and easier work to the dentist.
This 3D model of the mouth can also serve as a mould. Effectively eliminating the middleman in the production of prosthetic teeth. The traditional process (still employed by 9/10 dentists) is to take a physical mould of the mouth and send to a prosthetics manufacturer. This means the patient has to wait weeks for his teeth to be ready. The new process is in-house 3D modelling and in-house 3D printing – the patient can get diagnosed and fitted with prosthetics in one visit!
Innovations lined up further down include using the laser not only for scanning but also for operation. For example, if the patient is due for a temporary filling removal, the scanner can identify the surface of the synthetic material and vaporize it with laser. A rapid-resolving spectrometer can pick up trace amounts calcium in the air surrounding the target, indicating a bone is reached and lasing should stop.
In an era where information is everything, we can simply not dismiss a new source of data and a new aspect to the oral cavity. The health and environmental benefits of avoiding ionizing energy and the radioactive materials that are used in the screening process are not negligible either.
And there shall be light.