 The standard for digital computed tomography (CBCT) is the DICOM format. This acronym stands for ‘Digital Information and Communications in Medicine” which is a term that describes the standardized coding of x-ray images.
The standard for digital computed tomography (CBCT) is the DICOM format. This acronym stands for ‘Digital Information and Communications in Medicine” which is a term that describes the standardized coding of x-ray images.
A DICOM file contains the x-ray image or series of images (e.g. in a CBCT study) and other patient related information that is selected from a ‘library’ of standardized terms (e.g. patient name, identification number, and acquisition modality to name a few).
The DICOM library is extensive and continually updated to reflect changing identification standards. DICOM files are fully encrypted at 128 bits and allow electronic communication over the WEB. Having a standardized format also allows for viewing of images regardless of the proprietary acquisition modality that was used to take the imaging study. This allows cross-vendor ‘Interoperability’ or connectivity.
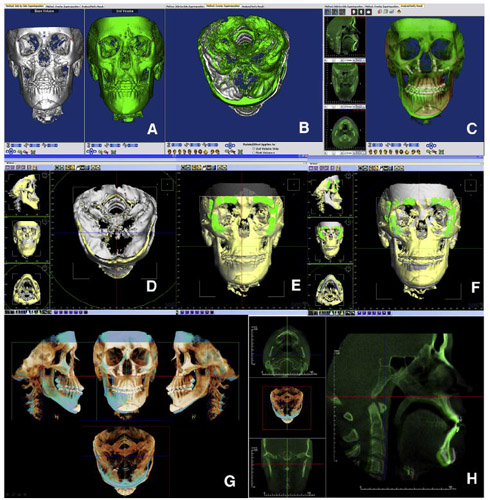
D Grauer, et al, in a review article published in the American Journal of Orthodontics Dentofacial Orthopedics, ( Am J Orthod Dentofacial Orthop. 2009) describe DICOM as it relates to CBCT images in orthodontics, the measurement of CBCT images, the creation of 2-dimensional radiographs from DICOM CBCT files, segmentation engines and multimodal images, the registration and superimposition of 3-dimensional images, special applications for quantitative analysis and 3D surgical prediction. They focus on three specific software packages which manage DICOM images: 3dMDvultus software (3dMD, Atlanta, Ga), Dolphin Imaging (Dolphin Imaging, Chatsworth, Calif) and InVivoDental (Anatomage, San Jose, Calif) although they do mention that there are other software packages and even freeware that are available to manage DICOM files.
Most sophisticated software applications allow for transforming images along different planes. They also allow visualization of a specific region of interest at different angles and the scaling of sections as desired. Typically there are multiple threshold filters for differentiating tissue density, clipping tools, and transparency filters for soft and hard tissues. As the authors of this article point out, rendering images for qualitative assessment is appropriate, but for quantitative assessment there are challenges with 3d rendering.
For instance, In terms of measurements, most landmarks visualized in 2d cannot be visualized or at the least are difficult to locate on a 3d surface that is curved. Another challenge is that a rendered image is impacted by many factors including contrast, movement during acquisition, the presence of metal, signal to noise ratio, and the threshold filters that have been applied by the operator. Thus, it is recommended that landmarks need to be located within a stack of slices. The authors report that with respect to accuracy and reliability of measurements on CBCT images there may be differences depending on the way landmarks are located within the slices. They suggest that ‘based on the available evidence….it is more accurate to locate landmarks in the stack of slices or on a segmented surface”
Also described is the creation of 2d radiographs from DICOM files. The authors state that measurements performed on these synthetic cephalograms from CBCT sections are, on average, similar to standard Cephs. However there may be an increase in landmark error calculation. Another facet of using multimodal images is in the different segmentation processes. The authors state that having a segmentation engine in the software to allow for distinguishing between the virtual surface and a rendered image is important because it permits the user to export anatomic models and the option of combining different modalities with the CBCT images (e.g. combining digital models through laser or optical scanners with the CBCT data).
The authors further describe the registration and superimposition of 3d images using the different software and the special applications associated with quantitative analysis including three-dimensional surgical prediction, one of the most promising aspect of this technology. Finally, the authors conclude that clinicians should be careful because the visual information garnered with these DICOM 3d software systems has not yet been linked to a diagnosis classification and that some of the available tools have not yet been validated with respect to accuracy and precision. They suggest that further research is needed in ‘the interpretation of orthodontic information from CBCT data’.
Submitted by Jeff Burgess DDS MSD
Editor in chief