The guideline emphasizes that periodontal care is an important component in controlling diabetes.
Diabetes affects approximately 285 million people worldwide, and this number is only expected to increase. Management of periodontal disease—which affects the gums and other supporting tissues around the teeth—can help reduce the risk of developing diabetes and can also help people with diabetes control their blood sugar levels. Studies have suggested there is a two-way relationship between diabetes and periodontal disease, and the IDF guideline outlines helpful guidance for health professionals who treat people living with and at risk for diabetes.
Health professionals should conduct annual inquiries for symptoms of periodontal disease such as swollen or red gums, or bleeding during tooth brushing; and to educate their patients with diabetes about the implications of the condition on oral health, and especially periodontal health. Everyone should maintain healthy teeth and gums to avoid periodontal disease, but people with diabetes should pay extra attention. Periodontal disease triggers the body’s inflammatory response which can affect insulin sensitivity and ultimately lead to unhealthy blood sugar levels. Establishing routine periodontal care is one way to help keep diabetes under control.
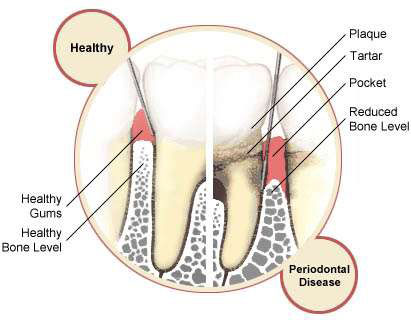 The Guideline on Oral Health for People with Diabetes should be released, and supports its encouragement of continued collaboration and communication between diabetes and oral healthcare professionals. Maintenance of proper oral hygiene for good oral health is an accepted part of the normal recommendations for a healthy lifestyle. Poor oral hygiene is associated with gingivitis, which can progress to more severe infection and inflammation leading to periodontitis. Infectious disease is known to be more common in people with diabetes if blood glucose control is poor, and inflammation is known to be associated with a decrease in insulin sensitivity and thus potentially a worsening of blood glucose control.
The Guideline on Oral Health for People with Diabetes should be released, and supports its encouragement of continued collaboration and communication between diabetes and oral healthcare professionals. Maintenance of proper oral hygiene for good oral health is an accepted part of the normal recommendations for a healthy lifestyle. Poor oral hygiene is associated with gingivitis, which can progress to more severe infection and inflammation leading to periodontitis. Infectious disease is known to be more common in people with diabetes if blood glucose control is poor, and inflammation is known to be associated with a decrease in insulin sensitivity and thus potentially a worsening of blood glucose control.
Both type 1 diabetes and type 2 diabetes carry a high burden of cardiovascular disease (CVD), and indeed it is the principal adverse outcome in type 2 diabetes. This is associated with increased levels of inflammatory markers which may or may not contribute to CVD, but are believed to do so in some other conditions such as rheumatoid arthritis, in which treatment of the inflammation appears to reduce the risk of CVD.
Recommendations on clinical care for people with diabetes:
1-Enquire annually as to whether each person with diabetes follows local recommendations for day-to-day dental care for the general population, and (where access permits) attends a dental professional regularly for oral health check-ups.
2 .Enquire at least annually for symptoms of gum disease (including bleeding when brushing teeth, and gums which are swollen or red.)
3 . In those people not performing adequate day-to-day dental care, remind them that this is a normal part of diabetes self-management, and provide general advice as needed. Advise those not attending for regular dental check-ups on the importance of doing so (where access permits)
4 . In those people with possible symptoms of gum disease, advise them to seek early attention from a dental health professional.
5- Education of people with diabetes should include explanation of the implications of diabetes, particularly poorly controlled diabetes, for oral health, especially gum disease.
In addition to helping increase awareness about the importance of oral care for people with diabetes, the guideline presents more opportunities for medicine and dentistry to work together. “I know that these clinical recommendations will be helpful for those professionals who work with and treat people with diabetes. I also encourage the medical and dental communities to work together to provide the best possible care for our patients.”
By Dr.Ali Hassan AlShehhi, DMD, Fujairah, UAE





 Guideline on Oral Health for People with Diabetes
Guideline on Oral Health for People with Diabetes